As a clinician with extensive experience in gastroenterology and a content strategist dedicated to educating patients and caregivers, I often encounter a common concern: “Could my eating habits be damaging my oesophagus?” The straightforward answer is yes.
The choices we make regarding food and how we consume it significantly impact oesophageal health over the years. The good news is that our everyday dietary decisions can also play a protective role, promoting comfort and overall well-being in this crucial part of our digestive system.
This article aims to speak directly to you—whether you are a patient, caregiver, or someone invested in health—to shed light on how eating habits affect oesophageal health over time, highlight warning signs to be vigilant about, and offer practical changes towards enhancing your comfort and long-term wellness.
The Importance of Daily Oesophageal Care
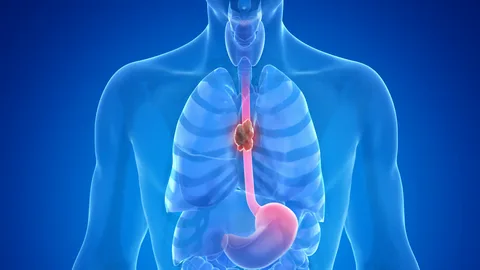
The oesophagus serves a vital function in our bodies, acting as the muscular tube that transports food and liquids from the mouth to the stomach. Each swallow relies on coordinated muscle contractions and a fragile lining that endures various challenges, including heat, acidity, and diverse textures. When our eating habits repeatedly stress this lining or interfere with its functioning, irritation and damage can accumulate over time.
Often, issues may not manifest immediately. Many conditions affecting the oesophagus develop subtly, with mild symptoms that are easy to overlook. Over time, these small signals can escalate into persistent discomfort, difficulty swallowing, or chest pain that disrupts daily meals and diminishes quality of life.
How Your Food Choices Influence Oesophageal Health
Portion Size and Meal Volume
Overindulgence in food can stretch the oesophagus and increase pressure at the lower oesophageal sphincter— a valve separating the oesophagus from the stomach. Consistently eating large portions heightens the risk for acid reflux and heartburn, leading to long-term inflammation.
Conversely, opting for smaller, balanced meals allows the oesophagus sufficient time to clear food efficiently. This simple shift can reduce burning sensations, minimize regurgitation, and promote a more comfortable post-meal feeling.
Eating Speed and Chewing Habits
Rushing through meals places added strain on the oesophagus. Inadequately chewed food typically travels as larger pieces, which can irritate the lining and hinder movement. Over the years, this habit can exacerbate swallowing discomfort.
By slowing down, chewing thoroughly, and placing utensils down between bites, you can facilitate smoother food movement through the oesophagus. Many patients find that practicing mindful eating diminishes chest tightness and alleviates the sensation of food getting stuck.
Temperature of Foods and Drinks
Hot foods and beverages can irritate the delicate lining of the oesophagus. Persistent exposure to high temperatures raises the risk of chronic inflammation. Allowing meals and drinks to cool slightly can protect fragile tissues and decrease irritation.
The Impact of Acid Exposure and Irritation
Acid Reflux and Eating Patterns
Chronic acid reflux is a prevalent threat to oesophageal health. Engaging in late-night eating, lying down soon after meals, or consuming trigger foods can amplify acid exposure.
Common trigger foods include:
- Fried or fatty dishes
- Chocolate and peppermint
- Tomatoes and citrus fruits
- Caffeinated beverages and alcohol
Reducing portion sizes in the evening and waiting a few hours between dinner and bedtime can often ease symptoms.
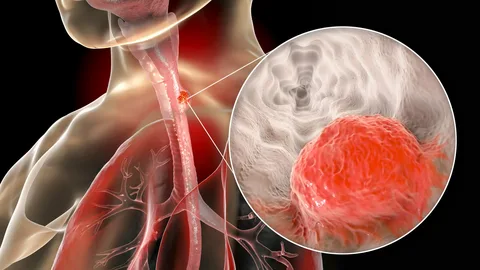
The Consequences of Chronic Reflux
Repeated acid contact can inflame the oesophageal lining and may lead to conditions such as oesophagitis or narrowing of the oesophagus. As the situation progresses, swallowing can become painful or increasingly difficult. If you currently experience reflux symptoms, it’s crucial to tweak your eating habits alongside following medical advice.
The Significance of Food Texture
Hard, Dry, and Abrasive Foods
Consuming dry bread, tough meats, or abrasive items can irritate the oesophagus, especially if swallowing is already an issue. Long-term irritation may heighten sensitivity.
Incorporating moisture through sauces, gravies, or soups helps food slide down smoothly, reducing friction.
Oesophagus-Friendly Food Choices
Opt for soft, comforting foods such as:
- Porridge and soft cereals
- Yogurt and smooth dairy alternatives
- Mashed vegetables
- Stewed fruits
- Well-cooked grains
These textures protect the lining and ease pressure on the oesophageal muscles.
The Role of Hydration in Comfort
Staying well-hydrated promotes saliva production, aiding in clearing food from the oesophagus. Insufficient hydration can lead to dryness, escalating any discomfort during swallowing.
Regularly sipping water, particularly during meals, can enhance the swallowing experience. Many individuals note improvement simply by consistently increasing their fluid intake.
Eating Habits Affecting Oesophageal Muscle Function
Regular Meal Timing
Irregular eating habits can disrupt the normal functioning of the oesophagus. Skipping meals followed by large food intake may overwhelm muscle coordination.
Establishing consistent meal times fosters predictable contractions, enhancing food clearance.
Alcohol and Muscle Control
Alcohol relaxes the lower oesophageal sphincter, increasing the risk of acid reflux while also irritating the lining directly. Limiting intake can help maintain muscle tone and reduce inflammation.
Weight and Oesophageal Pressure
Extra weight around the abdomen increases pressure on the stomach, which can force acid upward. Over time, this pressure contributes to reflux and discomfort.
Balanced eating patterns that promote gradual weight management can lower strain on the oesophagus and help maintain symptom control.
Recognizing Warning Signs of Potential Harm
Be alert to signals that may arise during or post-meals, including:
- Chronic heartburn
- Chest discomfort related to swallowing
- A sensation of food getting stuck
- A recurring cough after eating
- Pain when consuming hot or spicy foods
If these symptoms persist, adjustments to your diet should be made promptly, along with seeking medical guidance.
Tailoring Eating Habits to Specific Conditions
Achalasia and Food Implications
For conditions like achalasia that impact oesophageal muscle movement, eating habits become even more critical. Smaller portions, soft textures, and careful meal timing can alleviate discomfort.
Individuals may explore supportive methods, such as natural remedies in tandem with professional care or practical home remedies focusing on gentle eating practices.
Supplements and Digestive Support
Some may consider incorporating dietary supplements as part of a wellness plan, recognizing that they should complement, not replace, medical advice and healthy eating habits.
Developing Long-Term Protective Patterns for Oesophageal Health
Building Balanced Meals
Aim to create meals that incorporate lean proteins, soft carbohydrates, healthy fats, and fiber. A balanced diet can facilitate smoother digestion and minimize reflux triggers.
Respecting Posture During Meals
Maintaining an upright position while eating and remaining seated afterward allows gravity to assist in food movement. Avoid slouching or lying flat soon after your meals to enhance comfort.
The Emotional Influence on Eating and Symptoms
Stress affects digestion. Meals taken in anxious or hurried conditions can create muscle tension and disrupt normal swallowing. Creating a calming atmosphere for meals can greatly enhance oesophageal comfort.
Mindful eating techniques, such as taking slow breaths before beginning to eat, may reduce the frequency of symptom flare-ups over time.
Supporting Oesophageal Health Across Life Stages
Childhood and Early Practices
Healthy habits established in childhood often persist into adulthood. Encouraging young ones to chew properly, eat at a moderate pace, and minimize acidic drink consumption lays the foundation for long-term oesophageal health.
Midlife Adjustments
As people reach midlife, they may notice a rise in reflux symptoms. This period offers a chance to reassess portion sizes, alcohol habits, and evening routines.
Considerations in Older Age
In advancing years, changes in oesophageal muscle strength can occur. Focusing on soft food textures, staying hydrated, and maintaining regular meal times becomes increasingly vital.
Practical Steps to Start Today
You don’t need to make drastic changes to support your oesophageal health. Begin with manageable steps:
- Gradually reduce portion sizes
- Slow your eating pace
- Limit late-night meals
- Choose softer food textures when discomfort arises
- Increase your daily water intake
Consistency in these practices can be far more effective than aiming for perfection.
When Professional Guidance is Important
While dietary changes benefit many, ongoing symptoms should prompt a medical evaluation. Persistent swallowing difficulty, unexpected weight loss, or chest pain warrants immediate attention.
Combining thoughtful eating habits with clinical care optimizes your chances for long-term comfort and well-being.
Concluding Thoughts
The habits surrounding your eating can significantly shape your oesophageal health over time. Each meal provides signals to the muscles and linings responsible for transporting food to the stomach. By making mindful choices about portion sizes, respecting food textures, ensuring proper hydration, and adopting careful eating practices, you reinforce this vital pathway daily.
You wield more influence over your oesophageal health than you may realize. Through informed decisions and steady practices, you can minimize irritation, enhance swallowing comfort, and safeguard the health of your oesophagus for years to come.