Turning 40 is a milestone that brings wisdom, confidence, and life experience—but it also marks a significant shift in fertility. Women over 40 represent the fastest-growing demographic seeking fertility treatment, as modern society increasingly delays childbearing for careers, financial stability, or finding the right partner.
While IVF has revolutionized reproductive medicine, the reality is that age-related fertility decline presents substantial challenges that even advanced technology cannot completely overcome. Understanding the specific obstacles women over 40 face, realistic success rates, available strategies to optimize outcomes, and when alternative paths might be appropriate empowers you to make informed decisions about your fertility journey with eyes wide open to both possibilities and limitations.
The Biology of Age-Related Fertility Decline
Understanding why age affects fertility so dramatically helps contextualize the challenges:
Egg Quantity Decline:
Women are born with approximately 1-2 million eggs, declining to about 300,000 by puberty and continuing to diminish throughout life. By age 40, only about 3-5% of the original egg reserve remains.
Ovarian Reserve Markers:
- AMH (Anti-Müllerian Hormone): Typically <1.0 ng/mL by 40
- Antral Follicle Count: Usually fewer than 10 follicles
- FSH (Follicle Stimulating Hormone): Often elevated (>10-15 mIU/mL)
Egg Quality Decline:
More significantly than quantity, egg quality deteriorates with age. The mechanisms include:
Chromosomal Abnormalities (Aneuploidy): The percentage of eggs with wrong number of chromosomes increases dramatically:
- Age 30: 30-35% abnormal
- Age 35: 40-45% abnormal
- Age 40: 60-70% abnormal
- Age 42: 75-85% abnormal
- Age 44+: 90%+ abnormal
This happens because the cellular machinery controlling chromosome division degrades over time, leading to eggs with too many or too few chromosomes.
Mitochondrial Dysfunction: Eggs require enormous energy for fertilization and early development. Aging mitochondria (the cell’s powerhouses) become less efficient, reducing developmental potential.
Spindle Defects: The spindle apparatus that separates chromosomes during division becomes less reliable with age.
Oxidative Damage: Cumulative exposure to oxidative stress over decades damages cellular components.
Reduced Pregnancy Rates: Even when chromosomally normal embryos are available, implantation rates decline slightly with age due to changes in the uterine environment.
Increased Miscarriage Risk: Chromosomal abnormalities cause most first-trimester losses, making miscarriage rates rise sharply:
- Age 35: 15-20% miscarriage rate
- Age 40: 25-35% miscarriage rate
- Age 42: 35-45% miscarriage rate
- Age 45+: 50%+ miscarriage rate
Realistic IVF Success Rates After 40
Setting appropriate expectations is crucial for emotional preparedness:
Age-Specific Success Rates (Live Birth per Cycle):
Age 40:
- Success rate per cycle: 15-25%
- With own eggs and embryo transfer
- Varies significantly by individual circumstances
Age 41:
- Success rate per cycle: 10-20%
- Marked decline from even one year earlier
Age 42:
- Success rate per cycle: 5-15%
- Substantial drop in probability
Age 43:
- Success rate per cycle: 3-10%
- Success becomes increasingly unlikely
Age 44:
- Success rate per cycle: 1-5%
- Very low probability with own eggs
Age 45+:
- Success rate per cycle: <1-2%
- Extremely rare success with own eggs
Important Considerations:
Individual Variation: Some women over 40 have excellent ovarian reserve and egg quality, achieving higher success rates, while others face even steeper challenges.
Clinic Differences: Top centers with advanced laboratories may achieve slightly better outcomes, but age effects remain dominant.
Cumulative Rates: Multiple cycles improve cumulative chances, though success remains limited compared to younger ages.
PGT-A Impact: Genetic testing can identify chromosomally normal embryos when they exist, but can’t create them if none are present.
When consulting with a reputable IVF center in Jaipur, request age-specific success rates for your exact age, as even single-year differences matter significantly after 40.
Specific Challenges for Women Over 40
Poor Ovarian Response: Many women over 40 respond poorly to stimulation medications, producing few eggs per cycle:
- 3-5 eggs retrieved (vs. 10-15 in younger women)
- Higher medication doses required
- Extended stimulation periods
- Cycle cancellations due to inadequate response
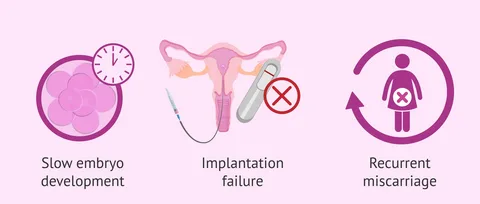
Fewer Eggs, Fewer Chances: When retrieval yields only 2-4 eggs, and 60-90% are chromosomally abnormal, the mathematics become challenging. Often no normal embryos result from a single cycle.
Extended Time to Success: Due to lower success rates, women over 40 typically need multiple IVF cycles to achieve pregnancy, requiring:
- Significant time investment (6-12+ months)
- Emotional endurance through repeated attempts
- Financial resources for multiple cycles
- Physical toll of repeated procedures
Higher Miscarriage Rates: Even after achieving pregnancy, first-trimester loss is common due to chromosomal abnormalities missed by PGT-A or embryos that test normal but have other developmental issues.
Pregnancy Complications: Women over 40 who successfully carry pregnancies face higher risks of:
- Gestational diabetes
- Preeclampsia
- Placental complications
- Cesarean delivery
- Preterm birth
- Low birth weight
However, with proper prenatal care, the majority of pregnancies result in healthy babies.
Emotional Toll: The combination of lower success rates, longer timelines, and higher loss rates creates significant emotional burden, requiring robust support systems.
Strategies to Optimize Success After 40
While age effects can’t be eliminated, certain strategies may improve outcomes:
Pre-Treatment Optimization
Comprehensive Testing:
- Ovarian reserve assessment (AMH, FSH, AFC)
- Thyroid function (TSH, antibodies)
- Vitamin D levels (deficiency common and correctable)
- General health screening
- Partner’s semen analysis
Supplements (Start 3+ Months Before):
CoQ10 (Ubiquinol form): 400-600mg daily
- Powerful antioxidant supporting mitochondrial function
- Best evidence for improving egg quality
- Particularly important for women over 40
DHEA: 25mg 3 times daily (total 75mg)
- Androgen precursor may improve ovarian response
- Only for women with diminished ovarian reserve
- Monitor testosterone levels
- Start 2-3 months before IVF
- Not appropriate for all women
Melatonin: 3mg before bed
- Antioxidant protecting eggs from oxidative damage
- Improves sleep quality
- May enhance egg and embryo quality
Omega-3 Fatty Acids: 1000-2000mg daily
- Anti-inflammatory effects
- Supports egg quality
- Cardiovascular benefits
Vitamin D: 2000-4000 IU daily (if deficient)
- Critical for egg quality and implantation
- Test levels, supplementing to reach 40-60 ng/mL
Prenatal Vitamins with Methylfolate: Daily
- Folic acid prevents neural tube defects
- Methylfolate better absorbed than folic acid
Lifestyle Modifications:
Achieve Healthy Weight: BMI 19-25 ideal
- Even 5-10% weight loss if overweight improves outcomes
- Underweight women should gain appropriately
Mediterranean Diet: Anti-inflammatory, nutrient-dense eating pattern
Moderate Exercise: 30-60 minutes, 5-6 days weekly
- Avoid excessive high-intensity training
- Walking, swimming, yoga ideal
Stress Management:
- Meditation, mindfulness practices
- Counseling or therapy
- Support groups
- Adequate sleep (7-9 hours)
Eliminate Toxins:
- Stop smoking immediately (dramatically worsens outcomes)
- Minimize alcohol consumption
- Avoid environmental toxins
- Reduce caffeine (<200mg daily)
IVF Protocol Optimization
Aggressive Stimulation Protocols: Higher medication doses may recruit more eggs, though response is still limited by ovarian reserve.
Micro-dose Lupron Flare: Uses GnRH agonist to create initial FSH surge, sometimes improving response in poor responders.
Natural or Mini-IVF: For very poor responders, lower medication doses with more frequent cycles may be cost-effective, though success rates are lower per cycle.
Growth Hormone Supplementation: For some poor responders:
- Omnitrope, Saizen, or similar
- Started with stimulation medications
- May improve egg quality and embryo development
- Expensive addition (several thousand dollars)
- Evidence mixed but sometimes recommended
Testosterone Priming: Low-dose testosterone patches before stimulation may improve follicle recruitment in some protocols.
Embryo Banking Strategy
Given low numbers of eggs per cycle and high chromosomal abnormality rates, many specialists recommend:
Multiple Egg Retrievals: Perform 2-4 retrieval cycles before any transfers:
- Accumulate embryos across multiple cycles
- Send all embryos for PGT-A testing
- Transfer only chromosomally normal embryos
- Maximizes chance of having at least one normal embryo
Advantages:
- Identifies any normal embryos if they exist
- Avoids transferring abnormal embryos
- Provides realistic assessment of viability
Disadvantages:
- Significant time investment (4-8 months)
- Financial burden of multiple retrievals
- Emotional toll of multiple cycles without transfer attempts
- Risk of no normal embryos after all efforts
PGT-A is Essential: For women over 40, genetic testing is strongly recommended:
- High abnormality rates make morphology-based selection inadequate
- Transferring normal embryos significantly improves success per transfer
- Reduces miscarriage risk
- Prevents wasting time transferring embryos destined to fail
An experienced IVF hospital in Jaipur should discuss whether embryo banking is appropriate for your circumstances, considering your ovarian reserve, timeline, and financial resources.
When to Consider Donor Eggs
Donor eggs represent the single most effective intervention for women over 40:
Success Rates with Donor Eggs: 50-65% per cycle, regardless of recipient age
Why Such High Success: Young, healthy donors (typically 21-30 years old) provide:
- Chromosomally normal eggs (70-80% normal vs. 10-40% in women over 40)
- Better egg quantity
- Superior embryo quality
- Higher implantation rates
When to Consider Donor Eggs:
After Multiple Failed IVF Cycles: If 2-3 cycles with own eggs produced no normal embryos or transfers failed
Very Elevated FSH/Low AMH: When ovarian reserve testing indicates extremely diminished reserve
Age 44+: When own-egg success is statistically very unlikely (<5%)
Time Constraints: When you want to minimize time to pregnancy
Genetic Concerns: When known genetic conditions make own eggs problematic
Personal Choice: Some women prefer this path from the outset for higher success rates
Emotional Considerations:
The decision to use donor eggs is deeply personal and often emotionally complex:
Grief Process: Mourning the loss of genetic connection to your child Acceptance Journey: Finding peace with alternative path to parenthood Disclosure Decisions: Whether/when to tell child about donor conception Partner Dynamics: One partner genetic parent while other is not Social Reactions: Managing family and friend responses
Support Resources:
- Counseling specifically for donor conception
- Support groups (RESOLVE, Donor Conception Network)
- Literature on donor conception parenting
- Time to process before making final decision
Many women who initially resist donor eggs later describe it as the best decision, allowing them to experience pregnancy and welcome their child without years of unsuccessful attempts.
Alternative and Complementary Approaches
Acupuncture: Some evidence suggests regular acupuncture may improve outcomes:
- Weekly sessions during IVF cycle
- Sessions before and after embryo transfer
- May reduce stress and improve blood flow
- Choose practitioners experienced in fertility treatment
Supplements Beyond Basics:
- Pycnogenol (pine bark extract) – antioxidant
- Resveratrol – mitochondrial support
- L-arginine – blood flow enhancement
- Alpha-lipoic acid – antioxidant
Discuss any supplements with your fertility specialist, as some may interact with medications.
Traditional Chinese Medicine: Some patients incorporate herbal medicine, though evidence is limited and safety with IVF medications must be considered.
Mind-Body Programs: Stress reduction interventions may improve outcomes:
- Mindfulness-based stress reduction
- Fertility yoga
- Guided imagery
- Relaxation techniques
Financial Realities
IVF after 40 often requires multiple cycles, creating significant financial burden:
Cost Considerations:
- Single cycle: $15,000-25,000 including medications
- Multiple cycles needed: $30,000-75,000+ common
- PGT-A testing: Additional $3,000-7,000 per cycle
- Supplements and adjunct treatments: $200-500 monthly
- Time off work for appointments and procedures
Financial Planning Strategies:
- Multi-cycle packages (if available and appropriate)
- Medical loans or payment plans
- Employer fertility benefits (increasingly common)
- Grants and financial assistance programs
- Health Savings Accounts for tax benefits
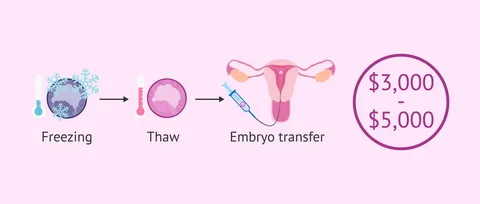
Donor Egg Costs:
- Fresh donor cycle: $25,000-40,000+
- Frozen donor eggs: $15,000-25,000
- Higher upfront cost but better success rates
- May require fewer cycles overall
Cost-Benefit Analysis: Discuss frankly with your specialist:
- Realistic assessment of own-egg success probability
- Expected number of cycles needed
- Total anticipated costs with own eggs
- Compare to donor egg costs and timelines
- Consider emotional and time costs alongside financial
Knowing When to Stop
One of the most difficult decisions is determining when to stop pursuing own-egg IVF:
Indicators It May Be Time:
- Multiple cycles (3-5+) producing no normal embryos
- Continued poor ovarian response despite protocol optimization
- Emotional exhaustion overwhelming life quality
- Financial resources depleted
- Time passed (age now 44-45+)
- Partner unable to continue
- Medical contraindications developing
Alternative Paths Forward:
- Donor eggs (experiencing pregnancy and motherhood)
- Embryo adoption (less expensive donor option)
- Traditional adoption
- Child-free living
There’s No “Right” Answer: The decision is deeply personal, balancing:
- Hope vs. reality
- Desire for genetic child vs. desire to be a parent
- Emotional resilience remaining
- Financial resources available
- Time and age factors
- Relationship considerations
Professional Guidance: Work with counselors experienced in fertility treatment to process this decision without judgment.
Success Stories and Realistic Hope
While statistics are sobering, success does occur:
- Some women over 40 have excellent egg quality despite age
- Persistent patients attempting multiple cycles sometimes succeed
- Each cycle provides only probability—individuals beat odds regularly
- Technological advances continue improving outcomes
However, Maintain Perspective:
- Individual success stories don’t change overall statistics
- Plan realistically while hoping optimistically
- Consider alternatives before resources (emotional, financial, time) are exhausted
- Success at any age requires both medical excellence and good fortune
Questions to Ask Your Specialist
- What are realistic success rates for someone my exact age with my ovarian reserve?
- How many cycles would you recommend attempting with own eggs?
- Would you recommend embryo banking?
- What protocol would you suggest?
- Should I consider growth hormone?
- When would you recommend considering donor eggs?
- What are costs for multiple cycles?
- What’s your experience treating women over 40?
Taking Action After 40
Move Quickly: Every month matters when egg quality is declining rapidly. Don’t delay evaluation and treatment.
Comprehensive Testing: Understand your specific situation before starting treatment.
Realistic Expectations: Acknowledge statistics while maintaining hope.
Financial Planning: Budget for likely multiple cycles or alternatives.
Emotional Support: Build support systems before starting.
Partner Communication: Ensure both partners understand challenges and are aligned on approach.
Time Limits: Set boundaries on how long you’ll pursue own-egg treatment.
Stay Informed: Understand all options including alternatives.
Conclusion
IVF after 40 is possible but challenging. Age-related egg quality decline creates substantial obstacles that even the best medical care can’t fully overcome. Success rates are significantly lower than for younger women, multiple cycles are typically required, and many women ultimately succeed only through donor eggs or other alternatives.
However, understanding these realities doesn’t mean abandoning hope—it means approaching your journey with informed expectations, optimizing every controllable factor, working with experienced specialists, and remaining open to alternative paths if own-egg attempts prove unsuccessful.
Whether success comes through your own eggs after persistent efforts, through donor eggs allowing you to experience pregnancy, through adoption completing your family, or through finding fulfillment in child-free living, you have options. The key is making informed decisions based on realistic assessments, giving yourself the best possible chance while protecting your emotional and financial wellbeing, and knowing when the most loving thing you can do for yourself is to embrace a different path to the life you deserve.