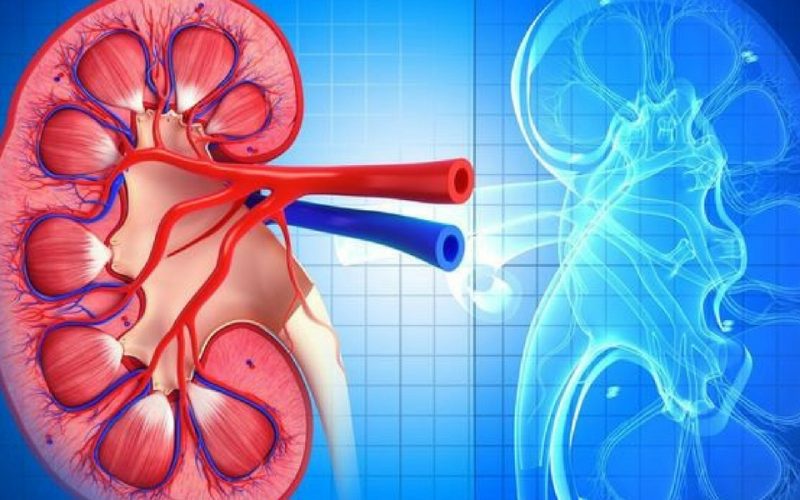
Lupus nephritis (LN) stands as one of the most severe complications of systemic lupus erythematosus (SLE), a complex autoimmune disorder affecting multiple systems in the body. Renal involvement, witnessed in roughly half of SLE cases, presents significant challenges in management and prognosis. Recent research, as published in Rheumatology (Oxford), sheds light on crucial aspects of LN, its histologic classification, long-term outcomes, and predictors of progression to chronic kidney disease (CKD).
Histologic Classification of Lupus Nephritis
The classification of LN, crucial for treatment decisions and prognostication, often relies on renal biopsy findings. In this recent study, patients were categorized into distinct groups based on their renal biopsy results:
- Proliferative LN (PLN) encompassed LN Class III and IV.
- Membranous LN (MLN) constituted LN Class V.
- Mixed LN comprised a combination of Class III or IV with Class V.
This classification allows for tailored management approaches, considering the varying pathologic mechanisms and prognostic implications associated with different LN classes.
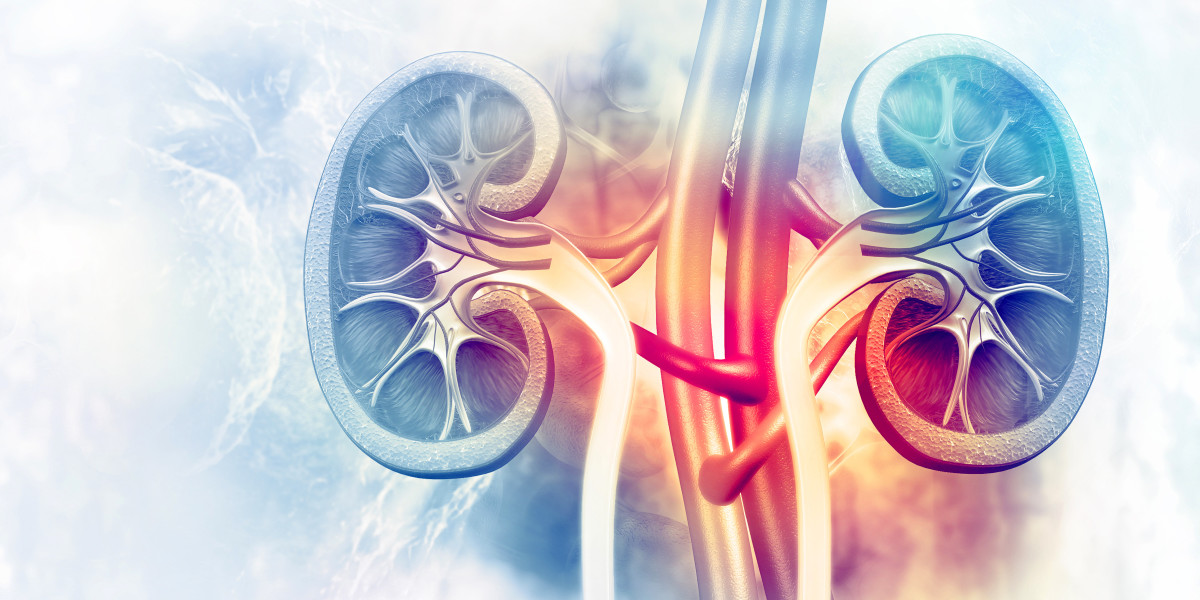
Clinical Manifestations and Long-Term Outcomes
Analyzing data from the nationwide Rheumatic Disease Portuguese Registry, researchers explored the clinical and laboratory manifestations of PLN and MLN, alongside their long-term outcomes. Over a median follow-up period of eight years, they observed distinct characteristics between PLN and MLN:
- Patients with MLN exhibited lower serum creatinine levels compared to PLN counterparts.
- Proteinuria levels, a hallmark of renal involvement, showed no significant difference between PLN and MLN groups.
- Complement levels were typically decreased in PLN cases, contrasting with near-normal levels in MLN.
Predictors of Progression to Chronic Kidney Disease
One of the critical findings of this study was the identification of predictors for progression to CKD. While proteinuria levels did not reliably predict LN histologic class, an estimated glomerular filtration rate (eGFR) cutoff of 75 mL/min/1.73 m2 after one year of treatment emerged as a robust predictor of CKD progression. Patients with an eGFR at or below this threshold faced a significantly heightened risk of developing CKD, emphasizing the importance of close monitoring and timely intervention in LN management.
Clinical Implications and Future Directions
The insights gleaned from this study carry significant implications for the clinical management of LN. Early identification of histologic class through renal biopsy aids in tailoring treatment strategies, with aggressive immunosuppression warranted in cases of ongoing active disease. Additionally, vigilant monitoring for disease flares is essential to mitigate further loss of renal function.

Moreover, the study underscores the need for further multicenter research to validate long-term outcomes in LN, especially in the context of proliferative and membranous classes. Addressing the limitations of small sample sizes and the retrospective nature of data collection will be critical in advancing our understanding of LN pathogenesis and refining treatment approaches.
Conclusion
Lupus nephritis represents a significant challenge in the management of systemic lupus erythematosus, with profound implications for patient outcomes. Recent research provides valuable insights into the histologic classification, clinical manifestations, and long-term outcomes of LN. Furthermore, the identification of predictors for progression to chronic kidney disease underscores the importance of early intervention and close monitoring in LN management. Moving forward, continued research efforts are essential to further elucidate the complex mechanisms underlying LN and improve patient outcomes.