Introduction
Lung cancer is the leading cause of cancer death in the United States, accounting for more deaths than breast, prostate, and colon cancer combined. Despite its prevalence, lung cancer screening rates remain alarmingly low, with fewer than 1 in 5 eligible Americans up to date with their screenings.
This article aims to highlight the importance of lung cancer screenings, discuss the barriers to accessing screenings, and provide recommendations for increasing screening rates to save lives.
Benefits of Lung Cancer Screenings
Lung cancer screenings are a valuable tool for detecting lung cancer at its earliest stages, when it is most treatable. Early detection has been shown to dramatically improve survival rates. Compared to those diagnosed with advanced lung cancer, patients diagnosed at an early stage have a more than 90% chance of surviving for at least five years.
Eligibility for Lung Cancer Screenings
According to the United States Preventive Services Task Force (USPSTF), adults between the ages of 50 and 80 who are current or former smokers with a history of at least 20 pack-years of smoking are eligible for annual lung cancer screenings. One pack-year is defined as smoking one pack of cigarettes per day for a year.
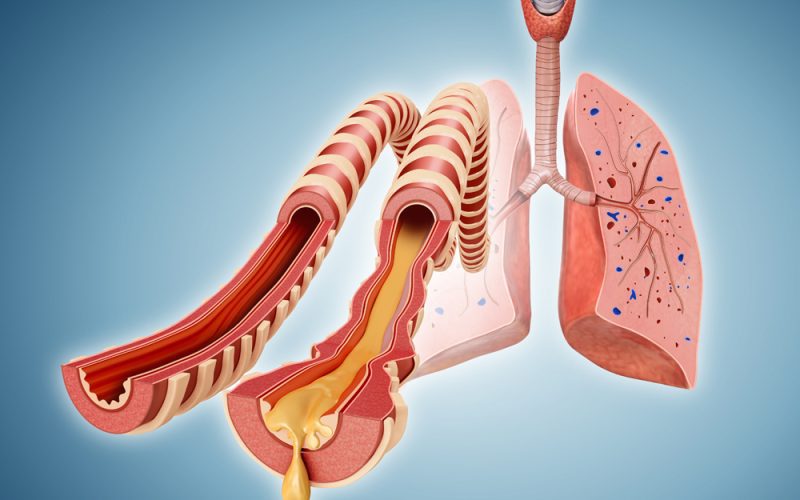
Types of Lung Cancer Screenings
The most common type of lung cancer screening is low-dose computed tomography (LDCT), a type of X-ray that provides detailed images of the lungs. LDCT screenings can detect small nodules or other abnormalities that may be indicative of lung cancer.
Other types of lung cancer screenings include chest X-rays, sputum cytology (microscopic examination of sputum), and bronchoscopy (a procedure that inserts a thin, flexible tube into the airways).

Barriers to Lung Cancer Screenings
Despite the proven benefits of lung cancer screenings, several barriers prevent eligible individuals from accessing these screenings:
- Lack of Awareness: Many people are unaware that they are eligible for lung cancer screenings or do not understand their importance.
- Stigma Associated with Smoking: Individuals who have smoked in the past or present may feel ashamed or embarrassed to discuss their smoking history with healthcare providers.
- Cost: Lung cancer screenings can be expensive, especially for uninsured or underinsured individuals.
- Access to Healthcare: Some individuals may not have access to healthcare facilities that offer lung cancer screenings.
- Fear of Radiation Exposure: LDCT screenings involve exposure to low levels of radiation, which may deter some individuals from getting screened.
Recommendations for Increasing Lung Cancer Screening Rates
To address the low lung cancer screening rates and improve early detection, several recommendations have been proposed:
- Public Awareness Campaigns: Public health campaigns should be launched to educate the public about the importance of lung cancer screenings and who is eligible.
- Provider Education: Healthcare providers should be educated about the benefits of lung cancer screenings and how to encourage eligible patients to get screened.
- Insurance Coverage: Insurance plans should cover lung cancer screenings for eligible individuals without cost-sharing requirements.
- Mobile Screening Units: Mobile screening units can be deployed to reach underserved communities and individuals with limited access to healthcare facilities.
- Smoking Cessation Programs: Smoking cessation programs should be integrated into lung cancer screening efforts to help individuals quit smoking and reduce their risk of developing lung cancer.
Conclusion
Lung cancer screenings are a crucial tool for detecting lung cancer at its earliest stages and saving lives. It is imperative to increase screening rates among eligible Americans to reduce the burden of lung cancer and improve the outcomes of those affected by this deadly disease.
By addressing the barriers to lung cancer screenings and implementing effective recommendations, we can ensure that more individuals have access to these screenings, improve early detection rates, and ultimately save lives from lung cancer.