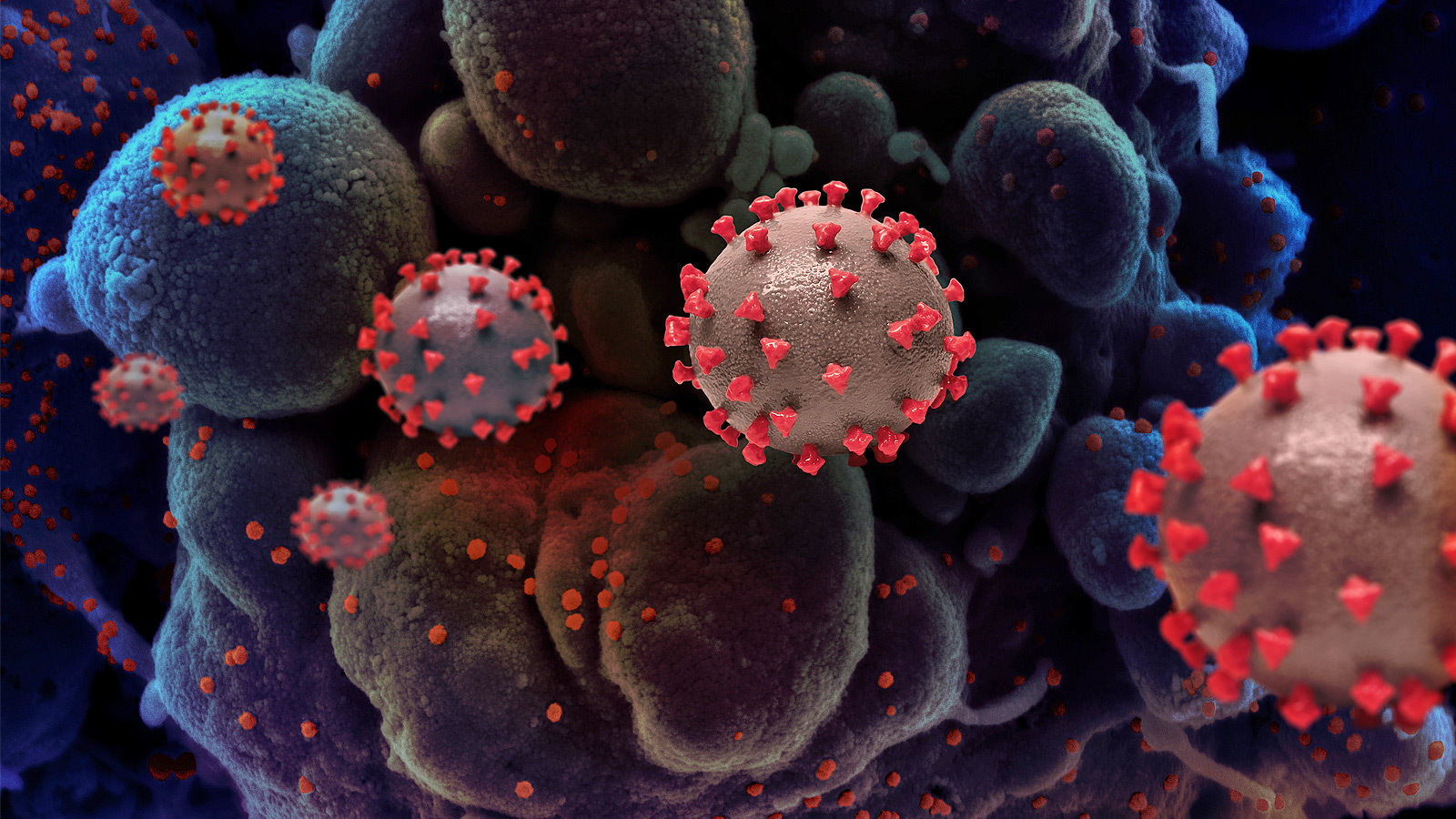
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, has indelibly altered the global health landscape. While the immediate impact of the virus has been widely documented, the long-term health consequences are still emerging. As we move further from the peak of the pandemic, it is crucial to understand how COVID-19 has influenced long-term health trends. This article delves into the COVID-19 long-term impact on various aspects of health, examining both direct and indirect consequences.
Long COVID: A Persistent Challenge
One of the most significant long-term impacts of COVID-19 is the condition known as “Long COVID” or post-acute sequelae of SARS-CoV-2 infection (PASC). Long COVID refers to a range of symptoms that persist for weeks or months after the acute phase of the infection has resolved. Common symptoms include fatigue, shortness of breath, cognitive dysfunction (often termed “brain fog”), and muscle pain.
Mechanisms and Risk Factors
The exact mechanisms underlying Long COVID are not fully understood, but several hypotheses exist. These include:
- Persistent Viral Infection: Some researchers believe that remnants of the virus may linger in the body, causing prolonged symptoms.
- Immune System Dysregulation: COVID-19 may trigger an overactive immune response, leading to chronic inflammation and autoimmunity.
- Organ Damage: The virus can cause direct damage to organs such as the lungs, heart, and brain, resulting in lasting health issues.
Risk factors for developing Long COVID include severe initial infection, older age, and preexisting health conditions. However, even young and previously healthy individuals can experience long-term symptoms.
Mental Health and COVID-19
The pandemic has also had a profound impact on mental health. Social isolation, economic uncertainty, and the fear of infection have contributed to increased rates of anxiety, depression, and other mental health disorders.
Long-Term Mental Health Trends
- Increased Prevalence of Mental Health Disorders: Studies have shown a significant rise in the prevalence of mental health disorders during the pandemic. This trend is likely to persist as the psychological impact of COVID-19 continues to unfold.
- Substance Abuse: The stress and uncertainty of the pandemic have led to increased substance abuse, including alcohol and drug use. This can have long-term consequences for both physical and mental health.
- Access to Mental Health Services: The pandemic has highlighted the need for accessible mental health services. Telehealth has emerged as a valuable tool, but disparities in access remain a challenge.

Impact on Chronic Diseases
COVID-19 has also affected the management and progression of chronic diseases. The pandemic disrupted routine healthcare services, leading to delays in diagnosis and treatment for conditions such as diabetes, hypertension, and cancer.
Long-Term Implications for Chronic Disease Management
- Delayed Diagnoses: Many individuals postponed medical appointments and screenings during the pandemic, resulting in delayed diagnoses and potentially worse outcomes for chronic diseases.
- Interrupted Treatment: Disruptions in healthcare services led to interruptions in treatment regimens for chronic conditions, which can exacerbate disease progression.
- Lifestyle Changes: Lockdowns and social distancing measures have impacted physical activity levels and dietary habits, contributing to the worsening of chronic diseases.
Cardiovascular Health
COVID-19 has been associated with a range of cardiovascular complications, including myocarditis, arrhythmias, and thromboembolic events. These complications can have lasting effects on cardiovascular health.
Long-Term Cardiovascular Impact
- Myocardial Injury: Studies have shown that COVID-19 can cause myocardial injury, which may lead to long-term cardiac dysfunction and heart failure.
- Increased Risk of Thrombosis: The virus can increase the risk of blood clots, leading to conditions such as deep vein thrombosis and pulmonary embolism. Long-term anticoagulation therapy may be required for affected individuals.
- Monitoring and Follow-Up: Survivors of severe COVID-19 may require ongoing monitoring and follow-up to manage cardiovascular complications.
Respiratory Health
Given that COVID-19 primarily affects the respiratory system, it is not surprising that long-term respiratory issues are a significant concern. Survivors of severe COVID-19 may experience lasting lung damage and reduced pulmonary function.
Long-Term Respiratory Impact
- Pulmonary Fibrosis: Some individuals develop pulmonary fibrosis, a condition characterized by scarring of the lung tissue, which can lead to chronic respiratory issues.
- Reduced Lung Function: Long-term studies have shown that survivors of severe COVID-19 may have reduced lung function, impacting their quality of life and ability to perform daily activities.
- Rehabilitation: Pulmonary rehabilitation programs can help improve lung function and overall health in individuals with long-term respiratory issues.
Neurological and Cognitive Effects
COVID-19 has been associated with a range of neurological and cognitive effects, including stroke, encephalitis, and cognitive impairment. These effects can have lasting consequences for survivors.
Long-Term Neurological Impact
- Cognitive Dysfunction: Many individuals with Long COVID report cognitive dysfunction, including memory problems and difficulty concentrating. This can impact daily functioning and quality of life.
- Neuropathy: Some individuals experience peripheral neuropathy, characterized by pain, numbness, and tingling in the extremities.
- Stroke and Encephalitis: COVID-19 can increase the risk of stroke and encephalitis, leading to long-term neurological deficits.
Conclusion
The COVID-19 long-term impact on health is multifaceted and far-reaching. From Long COVID and mental health challenges to the management of chronic diseases and cardiovascular complications, the pandemic has left an indelible mark on global health trends. As we continue to navigate the post-pandemic world, it is crucial to prioritize research, healthcare access, and support for those affected by the long-term consequences of COVID-19. Understanding and addressing these impacts will be essential for improving health outcomes and building resilience against future public health crises.