Modern Medicine: Transforming Healthcare in the 21st Century
Modern medicine is experiencing an exciting era of rapid advancements driven by technological innovations, scientific discoveries, and a more personalized approach to patient care. From AI-powered diagnostics to groundbreaking treatments in cancer, genetics, and mental health, the healthcare landscape is evolving in ways that offer new hope for patients and doctors alike. In this article, we explore the latest developments in modern medicine, examining their benefits, real-world applications, and case studies that demonstrate the transformative power of these innovations.
1. Artificial Intelligence and Machine Learning in Healthcare

Artificial intelligence (AI) is one of the most promising tools in modern medicine, offering a range of possibilities from diagnostics to treatment planning and patient care management. AI-powered tools and algorithms are transforming the way clinicians diagnose diseases, predict outcomes, and develop individualized treatment strategies.
Benefits of AI in Healthcare
AI offers several significant benefits:
- Increased Accuracy: AI algorithms can analyze medical data with precision, often detecting diseases that may be overlooked by human doctors.
- Time Efficiency: AI-driven systems process vast amounts of data quickly, allowing for faster diagnosis and reducing the time patients must wait for results.
- Cost Reduction: By automating routine tasks and improving the efficiency of healthcare delivery, AI can help reduce healthcare costs.
- Personalized Medicine: AI is crucial in tailoring treatments based on individual genetic, lifestyle, and environmental factors.
Examples of AI in Modern Medicine
- Radiology: AI models are now being used to interpret medical images. For example, Google Health’s AI system can detect breast cancer in mammograms with greater accuracy than radiologists. The system outperforms humans in distinguishing between benign and malignant tumors, leading to earlier diagnosis and treatment.
- Predictive Analytics: AI is being used to predict patient outcomes. For example, IBM Watson Health uses AI to predict the risk of diseases like heart failure by analyzing patient history, biomarkers, and other data.
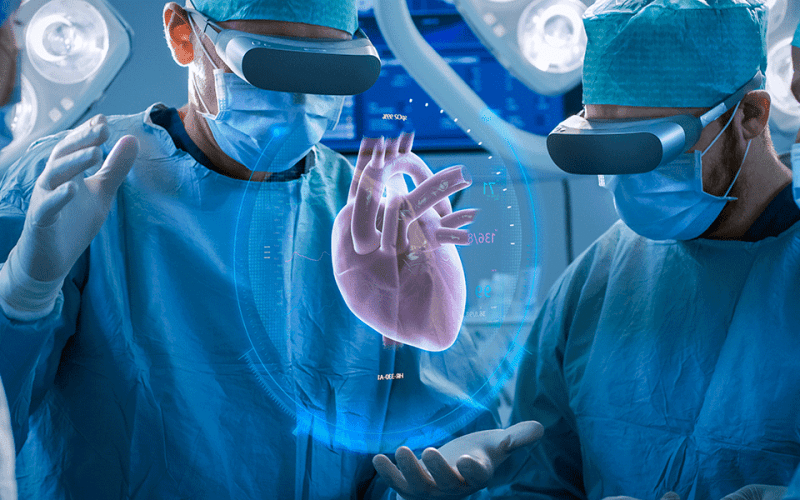
- Robotic Surgery: AI-guided robotic systems, such as the da Vinci Surgical System, help surgeons perform minimally invasive procedures with enhanced precision, reducing the risk of complications and improving recovery times.
Case Study: AI in Dermatology
A case study at Stanford University used AI to detect skin cancer. The AI system was trained using thousands of images of skin lesions to recognize patterns associated with melanoma. In tests, the AI system was able to identify skin cancer with an accuracy of 91%, compared to dermatologists’ accuracy rate of 88%. This highlights AI’s potential to assist in detecting cancers early, potentially saving lives.
2. Gene Editing and CRISPR Technology
Gene editing, particularly through CRISPR-Cas9, is a groundbreaking technique in modern medicine that allows for precise alterations of the DNA sequence. This has opened up new possibilities for treating genetic diseases, cancers, and even certain viral infections.
Benefits of Gene Editing
- Treatment of Genetic Disorders: Gene editing holds promise for treating inherited diseases such as sickle cell anemia, cystic fibrosis, and Duchenne muscular dystrophy.
- Cancer Therapies: CRISPR is being used to edit immune cells to target cancer more effectively, offering a new form of immunotherapy.
- Disease Prevention: In the future, gene editing could potentially be used to prevent genetic disorders by correcting mutations in embryos.
Examples of Gene Editing in Medicine
- Sickle Cell Anemia: In a landmark case, a patient suffering from sickle cell anemia was treated using CRISPR to edit their bone marrow cells. The edited cells were reintroduced into the patient, resulting in the patient being free from symptoms of the disease. This success represents a major step forward in using gene editing to treat genetic conditions.
- Cancer Immunotherapy: CRISPR is being used in CAR-T cell therapies, where T-cells are genetically modified to better target and destroy cancer cells. This approach has shown promise, particularly in treating blood cancers like leukemia and lymphoma.
Case Study: CRISPR and Sickle Cell Anemia
In 2020, a landmark case at the University of California, Berkeley, demonstrated the power of CRISPR in treating sickle cell anemia. The patient, who had previously undergone a bone marrow transplant, was treated with a CRISPR-based therapy. After several months, the patient showed no signs of sickle cell symptoms, marking a significant breakthrough in gene therapy.
3. Immunotherapy in Cancer Treatment
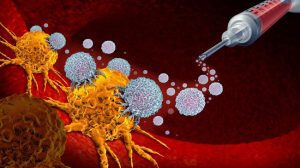
Immunotherapy, which enhances the body’s immune system to fight cancer, is one of the most promising treatments in modern oncology. By harnessing the immune system’s natural ability to identify and destroy cancer cells, immunotherapy offers a more targeted approach than traditional chemotherapy.
Benefits of Immunotherapy
- Targeted Treatment: Immunotherapies such as checkpoint inhibitors and CAR-T cell therapies specifically target cancer cells, reducing the side effects associated with traditional treatments like chemotherapy.
- Long-lasting Remission: Some patients who undergo immunotherapy experience long-term remission, even when their cancer is considered terminal.
- Less Invasive: Immunotherapies are typically less invasive than surgeries and offer an alternative to chemotherapy’s toxic side effects.
Examples of Immunotherapy in Action
- Checkpoint Inhibitors: Drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) block proteins on cancer cells that prevent the immune system from attacking them. These therapies have shown success in treating cancers like melanoma, non-small cell lung cancer, and kidney cancer.
- CAR-T Cell Therapy: Chimeric Antigen Receptor T-cell (CAR-T) therapy involves modifying a patient’s T-cells to recognize and attack cancer cells. The FDA approved Kymriah, a CAR-T therapy, for treating certain types of leukemia and lymphoma.
Case Study: CAR-T Therapy in Leukemia
One remarkable case of CAR-T therapy involves Emily Whitehead, a young girl diagnosed with acute lymphoblastic leukemia (ALL). After multiple rounds of chemotherapy failed, Emily underwent CAR-T therapy at the Children’s Hospital of Philadelphia. Her T-cells were modified to target her leukemia cells. Within weeks, she went into remission and remains cancer-free, showcasing the potential of immunotherapy to cure even aggressive cancers.
4. Telemedicine and Digital Health
The rise of telemedicine and digital health has transformed healthcare delivery, especially in the wake of the COVID-19 pandemic. Telemedicine allows patients to consult with healthcare providers remotely, reducing the need for in-person visits and expanding access to care, especially in rural and underserved areas.
Benefits of Telemedicine
- Improved Access to Healthcare: Patients in remote areas can consult specialists and receive treatment without needing to travel long distances.
- Convenience: Telemedicine provides patients with the ability to schedule appointments at their convenience, making healthcare more accessible.
- Cost-Effective: By reducing the need for hospital visits and in-person consultations, telemedicine helps reduce healthcare costs for both providers and patients.
Examples of Telemedicine in Practice
- Remote Consultations: Platforms like Teladoc and Doctor on Demand allow patients to consult with doctors via video calls, making it easier to receive treatment for minor illnesses, mental health issues, and chronic disease management.
- Wearable Devices: Devices like the Apple Watch and Fitbit now have features that allow users to track their health metrics, such as heart rate, ECG, and blood oxygen levels. These devices can sync data with healthcare providers, allowing for continuous health monitoring and timely interventions.
Case Study: Telemedicine During the COVID-19 Pandemic
During the COVID-19 pandemic, telemedicine usage skyrocketed as patients avoided in-person visits to reduce the risk of infection. A study from the Journal of the American Medical Association found that telehealth visits increased by 154% in March 2020 compared to the previous year. This shift highlighted the potential of telemedicine in providing continuous care during a global health crisis.
5. Regenerative Medicine and Stem Cell Therapy

Regenerative medicine is an emerging field focused on repairing or replacing damaged tissues and organs. Stem cell therapy and 3D bioprinting are key aspects of this field, offering innovative solutions for conditions that were once considered untreatable.
Benefits of Regenerative Medicine
- Tissue Regeneration: Stem cells can be used to regenerate damaged tissues and organs, potentially eliminating the need for transplants.
- Minimally Invasive: Many regenerative therapies are less invasive than traditional surgery, reducing recovery times and improving patient outcomes.
- Chronic Disease Management: Stem cell therapies have the potential to treat chronic conditions like osteoarthritis, heart disease, and neurological disorders.
Examples of Stem Cell Therapies
- Spinal Cord Injury: Clinical trials have shown that stem cells can help repair spinal cord injuries, offering hope for patients with paralysis.
- Heart Disease: Stem cells are being tested to regenerate heart tissue after heart attacks, potentially reversing damage and improving heart function.
Case Study: Stem Cell Therapy for Parkinson’s Disease
A recent clinical trial at the University of California, San Diego, explored the use of stem cells to treat Parkinson’s disease. Researchers implanted stem cells into the brains of patients with Parkinson’s to replace damaged neurons. Initial results showed that some patients experienced improvements in motor function, offering hope for future treatments.
6. Personalized Medicine and Precision Healthcare
Personalized medicine tailors medical treatment to an individual’s genetic makeup, environment, and lifestyle. By understanding the unique factors that influence how a patient responds to different treatments, personalized medicine promises more effective and targeted care.
Benefits of Personalized Medicine
- Optimized Treatment Plans: Personalized medicine allows doctors to select treatments based on genetic factors, improving their efficacy and minimizing side effects.
- Early Detection: Genetic testing can help identify individuals at risk for certain diseases, enabling earlier intervention and prevention strategies.
- Reduced Trial and Error: By understanding the genetic basis of diseases, doctors can avoid unnecessary treatments and find the most effective options from the start.
Examples of Personalized Medicine
- Pharmacogenomics: This branch of personalized medicine studies how a person’s genetic makeup affects their response to drugs. For instance, genetic testing can help determine whether a patient will respond well to specific cancer drugs, minimizing adverse reactions.
- Liquid Biopsy: Liquid biopsies allow doctors to detect genetic mutations in blood samples, offering a non-invasive method for diagnosing cancers and monitoring treatment progress.
Case Study: Precision Medicine in Cancer
In a case study published by the New England Journal of Medicine, a patient with advanced melanoma underwent genetic testing to identify mutations in his cancer cells. Based on the results, his treatment was tailored using targeted therapies, and the patient achieved significant tumor shrinkage. This case highlights how precision medicine can offer a more effective approach to cancer treatment.
Conclusion
Modern medicine is undergoing a revolution driven by technological advancements, scientific breakthroughs, and a focus on personalized, patient-centered care. From AI and gene editing to immunotherapy and regenerative medicine, the future of healthcare looks promising. These innovations are improving outcomes, reducing side effects, and opening up new possibilities for treating diseases once thought incurable.
As we continue to explore these emerging technologies and therapies, the healthcare landscape will continue to evolve, providing hope for better health and longer lives. However, as with any new technology, careful consideration of ethical, regulatory, and social implications is necessary to ensure that these advancements benefit all people, equitably and sustainably.