What Is Horner Syndrome?
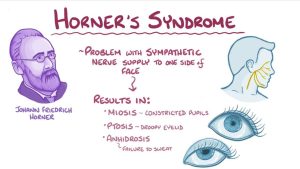
Horner syndrome, alternatively known as Horner-Bernard syndrome or oculosympathetic palsy, stands as a rare condition characterized by facial challenges arising from damaged nerves. This comprehensive exploration delves into the occurrence, symptoms, causes, diagnosis, and available treatments for Horner Syndrome.
Horner Syndrome Symptoms
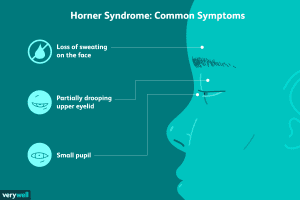
Recognizing Horner Syndrome involves understanding the distinctive signs affecting the eyes and face. Notable symptoms include:
- No sweat on one side of the face
- Droopy upper eyelid (ptosis)
- Slightly raised lower eyelid (inverse ptosis)
- Small pupil (miosis)
- Unequal pupil sizes (anisocoria)
- Pupil doesn’t open widely or is slow to open in dim light
- Sunken or bloodshot eye
Beyond these primary indications, additional symptoms may manifest, particularly in middle-aged men, such as pain or headaches. Furthermore, in children who develop Horner Syndrome before the age of 2, observable signs may include heterochromia iridis (one iris lighter than the other) and a lack of flushing on one side of their face on hot days or after physical activity.
Causes
The origins of Horner Syndrome are multifaceted, with approximately 35-40% of cases presenting an unknown cause. Possible factors contributing to this condition include genetic influences and damage to the nerve pathways that regulate eye function, heart rate, sweat, and blood pressure.
Three Distinct Pathways Involved:
- First order (central): This pathway encompasses nerves running from the hypothalamus in the brain to the chest, passing through the brain stem and spinal cord. Potential conditions affecting this pathway include sudden loss of blood to the brain stem, tumors on the hypothalamus, spinal cord lesions, stroke, and damage to myelin.
- Second order (preganglionic): Nerves extend from the chest to the top of the lungs and along the carotid artery in the neck. Contributing factors may include tumors in the upper lung or chest and injury or surgery to the neck or chest.
- Third order (postganglionic): This pathway runs from the neck to the middle ear and eye. Conditions impacting this route involve carotid artery lesions, middle ear infections, injury to the base of the skull, and certain types of headaches.
While neck or shoulder injuries during birth can exceptionally lead to Horner Syndrome in infants, it remains a rare occurrence. Additionally, babies born with damage to their aorta or neuroblastoma, a type of cancer, may also exhibit signs of Horner Syndrome.
Diagnosis
Diagnosing Horner Syndrome requires a thorough examination conducted by a healthcare professional, often an eye doctor (ophthalmologist). The process involves a physical exam, a detailed inquiry into medical history to identify potential sources of nerve damage, and pupil reaction tests facilitated by eye drops.
Moreover, imaging tests such as X-rays, magnetic resonance imaging (MRI), computerized tomography (CT) scans, and carotid ultrasounds may be employed to visualize any growth, damage, or injury contributing to Horner Syndrome. Blood or urine tests may also be recommended to identify underlying health problems associated with nerve damage.

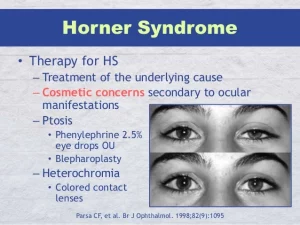
Treatment
Addressing Horner Syndrome involves managing the underlying health issues rather than targeting the syndrome itself. Specific treatments may include:
- Surgical removal: If a tumor or lesion is identified, surgical removal may be recommended.
- Radiation and chemotherapy: In cases where tumors are present, additional treatments such as radiation or chemotherapy may be pursued to address the condition comprehensively.
While there is no specific cure for Horner Syndrome, timely intervention and appropriate management of underlying health concerns can significantly alleviate its symptoms and enhance overall well-being.
Conclusion
In conclusion, Syndrome presents itself as a rare and intricate condition, impacting facial nerves and manifesting in distinct symptoms such as ptosis, miosis, and anisocoria. While the causes may remain elusive in a significant percentage of cases, potential factors include genetic influences and damage to intricate nerve pathways regulating various bodily functions.
Understanding the three distinct pathways involved—central, preganglionic, and postganglionic—offers insights into the diverse origins of Syndrome. From neurological conditions to physical injuries, the underlying causes can vary widely. Notably, it is crucial to recognize symptoms promptly, especially in children, as early intervention can be vital for effective management.












