Introduction
The intersection of COVID-19 and diabetes has emerged as a critical concern since the onset of the pandemic. Individuals with diabetes are deemed particularly vulnerable to severe complications if they contract the virus. Understanding the nuances of this relationship is paramount for effective management and mitigation strategies. In this comprehensive guide, we delve into the scientific insights regarding COVID-19 and diabetes, shedding light on crucial aspects that can help individuals navigate these challenging times with greater confidence and resilience. All You Need To Know About (arms And Legs Tingling)
Understanding Diabetes and its Implications
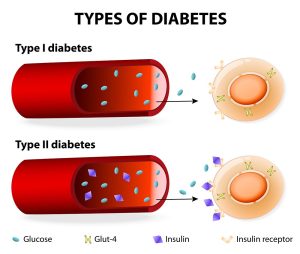
Diabetes is a chronic metabolic disorder characterized by elevated levels of blood glucose, either due to inadequate insulin production or the body’s ineffective use of insulin. This condition significantly compromises the body’s ability to regulate blood sugar levels, leading to various complications over time. Types of diabetes include type 1, type 2, and gestational diabetes, each with distinct underlying causes and management approaches.
Type 1 Diabetes
Type 1 diabetes, often diagnosed in childhood or adolescence, results from the immune system’s destruction of insulin-producing beta cells in the pancreas. Individuals with type 1 diabetes require lifelong insulin therapy to manage their condition effectively. Despite advancements in treatment modalities, maintaining optimal blood sugar control remains a daily challenge for those with type 1 diabetes.
Type 2 Diabetes
Type 2 diabetes, the most common form of diabetes, typically develops in adulthood and is closely linked to lifestyle factors such as poor diet, sedentary behavior, and obesity. In type 2 diabetes, the body becomes resistant to insulin or fails to produce enough insulin to meet its needs. While lifestyle modifications and oral medications are often prescribed as initial treatment measures, some individuals may eventually require insulin therapy to manage their condition effectively.
Gestational Diabetes
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased demands, leading to elevated blood sugar levels. While gestational diabetes usually resolves after childbirth, affected individuals are at a higher risk of developing type 2 diabetes later in life. Proper management, including dietary adjustments and monitoring blood sugar levels, is crucial to ensure the health of both the mother and the baby.
COVID-19 and Diabetes: A Complex Relationship
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, has posed significant challenges for individuals with diabetes. Emerging evidence suggests that diabetes not only increases the risk of contracting COVID-19 but also exacerbates the severity of the disease and contributes to poorer outcomes. Several factors contribute to this complex relationship:
Increased Susceptibility to Infection
Individuals with diabetes may experience weakened immune function, making them more susceptible to viral infections such as COVID-19. Moreover, the presence of underlying health conditions often associated with diabetes, such as obesity and cardiovascular disease, further heightens the risk of severe illness from COVID-19.
Impaired Immune Response
Diabetes can impair various aspects of the immune system, including inflammation regulation and immune cell function. This dysfunction may hinder the body’s ability to mount an effective immune response against viral pathogens like SARS-CoV-2, prolonging the duration and severity of illness.
Dysregulated Inflammation
Inflammation plays a crucial role in the progression of COVID-19, contributing to respiratory compromise and multi-organ dysfunction. Individuals with diabetes often exhibit chronic low-grade inflammation, which may exacerbate the inflammatory response triggered by SARS-CoV-2 infection, leading to more severe disease manifestations.
Impact on Metabolic Health
COVID-19 can disrupt metabolic homeostasis, leading to fluctuations in blood sugar levels even in individuals without preexisting diabetes. For those with diabetes, managing blood glucose becomes even more challenging during illness, as factors such as reduced food intake, increased stress hormone levels, and the use of certain medications can affect glycemic control.
Strategies for Mitigation and Management
Given the heightened risks faced by individuals with diabetes during the COVID-19 pandemic, proactive measures are essential to minimize exposure to the virus and optimize health outcomes. Here are some strategies recommended by healthcare experts:
Prioritize Vaccination
Vaccination against COVID-19 is strongly recommended for individuals with diabetes, as it can significantly reduce the risk of severe illness, hospitalization, and death. Both mRNA vaccines (e.g., Pfizer-BioNTech, Moderna) and viral vector vaccines (e.g., Johnson & Johnson’s Janssen) have been shown to be safe and effective in this population.
Maintain Optimal Blood Sugar Control
Achieving and maintaining target blood sugar levels is critical for reducing the risk of complications associated with both diabetes and COVID-19. Close monitoring of blood glucose, adherence to prescribed medications, and lifestyle modifications (e.g., healthy diet, regular exercise) can help individuals with diabetes manage their condition effectively.
Practice Preventive Measures
In addition to vaccination, individuals with diabetes should adhere to recommended preventive measures to reduce the risk of COVID-19 transmission, including wearing masks, practicing good hand hygiene, and maintaining physical distancing, especially in crowded or indoor settings.

Seek Timely Medical Care
Prompt medical attention is essential for individuals with diabetes who develop symptoms of COVID-19 or experience worsening glycemic control. Early intervention can help prevent the progression of illness and mitigate the risk of complications, including acute respiratory distress syndrome (ARDS) and organ failure.
COVID-19 Vaccines
| Vaccine | Type | Efficacy | Doses | Recommended Age |
|---|---|---|---|---|
| Pfizer-BioNTech | mRNA | 95% | 2 doses | 12 years and up |
| Moderna | mRNA | 94.1% | 2 doses | 18 years and up |
| Johnson & Johnson’s Janssen | Viral vector | 66.3% (in preventing moderate to severe COVID-19) | 1 dose | 18 years and up |
Conclusion
The relationship between COVID-19 and diabetes underscores the importance of comprehensive healthcare strategies tailored to the needs of individuals with underlying medical conditions. By understanding the intricate interplay between these two entities and implementing proactive measures for prevention and management, we can mitigate the impact of the pandemic on vulnerable populations and strive towards better health outcomes for all.
In conclusion, navigating the challenges posed by COVID-19 and diabetes requires a multifaceted approach encompassing education, prevention, and collaboration among healthcare stakeholders. By staying informed, prioritizing health-promoting behaviors, and seeking timely medical intervention when needed, individuals with diabetes can empower themselves to safeguard their well-being amidst the ongoing pandemic.












