Introduction
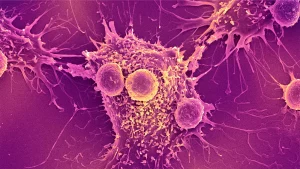
Insulinoma, an uncommon pancreatic tumor arising from endocrine cells, warrants a detailed examination. This article delves into its multifaceted aspects, including causes, diverse symptoms, diagnostic procedures, and a comprehensive overview of available treatments.
Who is Affected?
- Incidence Rates: With approximately 4 in 1 million people developing insulinomas, this condition is relatively rare.
- Age Profile: Typically diagnosed in individuals aged 40 to 50, emphasizing the importance of age-related considerations in diagnosis and management.

by: www.cosyfeet.com
Effects on the Body
- Insulin Overload: Insulinomas release excessive insulin, leading to a cascade of symptoms.
- Varied Symptoms: Explore symptoms like weakness, confusion, rapid heartbeat, loss of consciousness, and seizures.
Malignancy Risk
- Benign Nature: More than 90% of insulinomas are benign; however, a small percentage may become malignant.
- Potential Spread: Malignant insulinomas may spread to the liver or lymph nodes, but such occurrences are exceedingly rare.
Symptoms and Causes
- Associated Syndromes: Insulinoma is linked to inherited conditions, including MEN1, Von Hippel-Lindau syndrome, NF1, and TCS.
- Symptomatology: From hypoglycemia to seizures, grasp the diverse symptomatology associated with insulinomas.
Diagnosis and Tests
- Diagnostic Methods: Understand the diagnostic process, including blood glucose tests, CT scans, MRI, and endoscopic ultrasound.
- Grading Stages: Learn about grading stages, differentiating between low-grade, intermediate-grade, and high-grade tumors.

Management and Treatment
- Surgical Interventions: Explore surgical options, such as enucleation, partial pancreatectomy, and Whipple surgery.
- Alternative Treatments: Delve into alternative treatments like PRRT, targeted therapy, chemotherapy, and medications.
Complications
- Treatment Complications: Acknowledge the potential complications associated with pNET treatments, ranging from surgical complications to side effects of nonsurgical therapies.
- Discussion with Healthcare Provider: Engage in a thorough discussion with your healthcare provider to comprehend potential complications specific to your case.

Prevention
- Inherited Conditions: While direct prevention is challenging, recognize the association Treatment for other health Problems with inherited conditions.
- Monitoring Strategies: Adopt monitoring strategies, such as recognizing symptoms and understanding signs of low blood sugar.
Outlook / Prognosis
- Positive Outlook: With early diagnosis and surgical intervention, the prognosis for insulinoma is generally positive.
- Dietary Considerations: Explore dietary changes post-surgery and understand their role in long-term recovery.
Living With
- Post-Surgery Care: Learn about post-surgery care, including dietary adjustments and lifestyle modifications.
- Managing Symptoms: Understand strategies for managing common symptoms like fatigue and diarrhea.
When to Seek Medical Attention
- Emergency Situations: Recognize signs necessitating a visit to the emergency room, including severe shortness of breath, high fever, vomiting, or persistent diarrhea.
- Communication with Healthcare Provider: Know when to contact your healthcare provider regarding changes in symptoms, treatment side effects, or follow-up examinations.

Conclusion
Insulinoma, though rare, demands a comprehensive understanding of its nuances. From varied symptoms to intricate treatment options, this knowledge equips individuals to navigate their unique journey to recovery. Always consult healthcare professionals for personalized guidance and support.