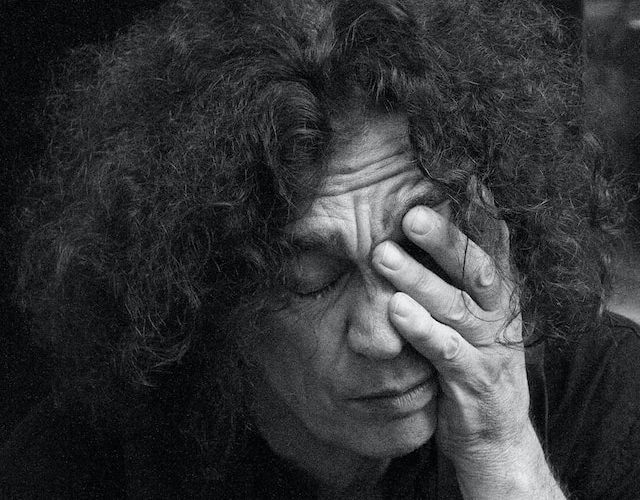
Introduction: Shingles, a painful and blistering rash caused by the varicella-zoster virus, is an all-too-familiar affliction for many. While most people recover from shingles without complications, there exists a rare but severe condition that can emerge in its aftermath: post-shingles encephalitis. In this article, we delve into the depths of this enigmatic disorder, exploring its risk factors and shedding light on the factors that contribute to its occurrence.
- Defining Post-Shingles Encephalitis: Post-shingles encephalitis is a condition characterized by inflammation of the brain and central nervous system following an episode of shingles. While the exact cause of this complication remains unclear, several risk factors have been identified.
- Age and Immune System: Age plays a significant role in determining the vulnerability to post-shingles encephalitis. Studies have shown that individuals over the age of 60 are at a higher risk of developing this condition. The immune system weakens with age, making it harder for the body to combat the reactivation of the varicella-zoster virus, which can then spread to the brain.
- Immunocompromised Individuals: Individuals with compromised immune systems, such as those with HIV/AIDS, cancer, or undergoing organ transplantation, face an increased risk of post-shingles encephalitis. Their weakened immune response allows the virus to flourish, potentially leading to severe complications.
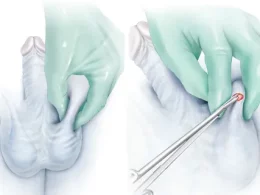
- Severity and Location of Shingles Rash: The severity and location of the shingles rash can also influence the likelihood of post-shingles encephalitis. Studies have suggested that individuals who experience a more extensive or severe rash are more prone to developing complications. Additionally, shingles involving the face and head, known as herpes zoster ophthalmicus, have been linked to a higher risk of encephalitis due to the proximity of the virus to the central nervous system.
- Genetic Factors: Emerging research indicates that certain genetic factors may predispose individuals to post-shingles encephalitis. Variations in the human leukocyte antigen (HLA) genes, responsible for regulating the immune response, have been associated with an increased susceptibility to neurological complications after a shingles infection.
- Timely Antiviral Treatment: Prompt treatment of shingles with antiviral medications, such as acyclovir, can help minimize the risk of post-shingles encephalitis. By reducing the viral load and duration of the infection, antiviral therapy may prevent the virus from reaching the brain and causing inflammation.
Conclusion: Post-shingles encephalitis remains a rare but serious complication that can occur after an episode of shingles. While the precise mechanisms behind its development are not yet fully understood, certain risk factors have been identified. Age, compromised immune systems, severity and location of the shingles rash, genetic factors, and timely antiviral treatment all play crucial roles in determining an individual’s susceptibility to this condition.
As further research unfolds, a clearer picture of post-shingles encephalitis will emerge. In the meantime, raising awareness about the risk factors can help healthcare professionals identify high-risk patients and implement preventive measures to mitigate the potential complications associated with this condition.